Lumbar Degenerative Disc Disease
Lumbar degenerative disc disease (DDD) is a common cause of low back pain. The vertebrae are cushioned by intervertebral discs which act as shock absorbers, for the spine. Over time, these natural shock absorbers wear out and degenerate due to aging, trauma or injury leading to DDD. Degenerative disc disease is not actually a disease but refers to the changes in the spine that occur as a part of the normal aging process.
Traumatic injury, aging, wear and tear, improper posture, repetitive movements, overuse, poor body mechanics and being overweight may alter the structure and function of the disc. All of these structural changes can place abnormal stress to your lower back causing pain.
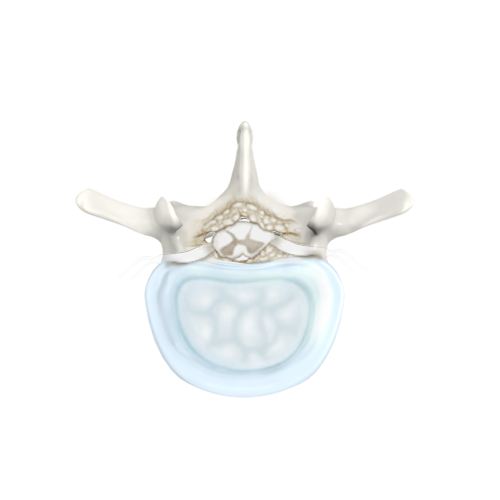
The normal intervertebral disc is composed of a nucleus pulposus, at the center, surrounded by a fibrous ring known as annulus fibrosus. The nucleus pulposus is a soft, well hydrated, jelly like substance that acts as a shock absorber. Over time, the nucleus pulposus begins to dehydrate and become stiff, failing to provide shock absorber action. This also lead to a reduction to the disc height, exerting excess stress over the surrounding annulus fibrosis, resulting in damage to the annulus which can cause instability of the lumbar spine and pain.
Symptoms
Some people are unaware of their condition and are usually informed about it on being examined for another health problem. Some individuals with lumbar DDD may not experience any symptoms, however when symptoms occur they develop gradually and worsen over time. Most patients with lumbar DDD will experience low back pain that radiates to the buttocks and legs and may aggravate with movement. Other symptoms include tingling or numbness in your legs, or difficulty walking, and rarely, loss of bowel and bladder control.
Diagnosis
Your physician will diagnose lumbar DDD depending on your symptoms, medical history and a physical and neurological examination. Your reflexes are tested and any muscle weakness, loss of sensation or other signs of neurological injury are noted. Diagnostic imaging tests such as X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans may be used to confirm the diagnosis. X-rays of the spine are taken to identify the collapsed disc space. A CT or MRI scan may be used to reveal disc and endplate changes. A discography may be performed to confirm the diagnosis. Discography is a diagnostic procedure where a contrast dye is injected into the affected disc to determine the damage and source of pain.
Treatment
Treatment of lumbar DDD comprises of non-surgical and surgical treatment options. The non-surgical treatment options such as anti-inflammatory and pain medications, muscle relaxants, physical therapy, spinal injections, certain types of braces, and acupuncture may help relieve the pain and other associated symptoms. Your doctor may combine two or more treatment modalities to enhance the success of the treatment.
Surgery may be necessary in patients with spinal instability or neurological dysfunction and persistent symptoms despite non-operative treatment. Spinal stabilization and fusion can be used to surgically treat lumbar DDD, which would help ease the pain and stabilize the spine.
Consult your doctor if you have any queries regarding lumbar DDD. Your doctor is a reliable source to answer all your questions and help you understand the condition better.










